Accidental bowel leakage (ABL) is a loss of normal control of bowels leading to leakage of stool (fecal incontinence) or leakage of stool and gas (anal incontinence). ABL is a common problem and about 6 percent of young women and about 15 percent of older women experience it during their lifetime.
ABOUT ABL
ABL can be upsetting and embarrassing. Many women find it hard to discuss with their doctors and nurses. It can feel as if you are the only one suffering from this problem. But it is common for women to experience these problems. By talking with your healthcare provider, you can find about causes and treatments. Depending upon the cause, these therapies may help you manage the leakage or – even cure your ABL.
The usual cause of ABL is a problem with the muscles or nerves in the rectum and anus. Normally, they work together to control bowel movements. Women with ABL, however, are not always able to control their bowel movements. Some women have difficulty controlling gas. Others have more severe symptoms such as loss of control of liquid or formed stool.
One of the biggest risks for ABL is injury to the anal sphincters during vaginal delivery. For example, the anal sphincter muscles may tear or be cut during a vaginal delivery. Even if the tear is repaired, damage to the bowel muscles and nerves can progress with time. As we age, our pelvic muscles weaken. Thus, bowel control problems can also occur later in life. Other factors that increase your risk for ABL include:
• Diabetes that is not in good control.
• Bowel problems such as irritable bowel syndrome, hemorrhoids, rectal prolapse, or anything that leads to diarrhea.
• Radiation therapy to the pelvic area.
• Nervous system disorders, such as multiple sclerosis, stroke, or spinal cord injury.
• Certain medications or nutritional supplements.
• Severe constipation.
DIAGNOSIS
Proper bowel control relies on a complex system of nerves and muscles and good gastrointesinal health. A careful review of your health history including all medications and supplements you take is needed to find the best treatment for you. Your health care provider will also ask about your vaginal childbirth experience, including how many children you have had, whether a forceps or vacuum was used, and any episiotomies or perineal tears you experienced.
The provider will examine your anal area and look for any injury. This starts with an examination of the skin surrounding the anus and a rectal exam. Your provider will look for signs of a fistula, which is a connection between the bowel and the vagina or the perineal skin.
You may need a series of tests to further evaluate the problem:
- Defecography: This imaging test is used to study your rectum and anal canal during a bowel movement using X-rays or MRI.
- Anoscopy or proctoscopy: A camera is used to look inside your anus or rectum.
- Anorectal manometry: The strength of your anal sphincter is tested by having you squeeze on a pressure-sensing probe.
- Nerve tests: These tests check if the nerves to your rectum and anus are working as they should.
- Ultrasound: This exam takes a picture from inside your rectum of the anal sphincter muscles. The doctor looks for any defects or weak areas in these muscles.
These tests are easy to do and important to help your provider understand the whole picture.
TREATMENTS
There are many treatment options. It may take a period of trial and error to find the one or combination of treatments that work best for you. Be honest with your provider and keep working to find a solution.
LEARN THE TERMS
- Accidental bowel leakage (ABL): Leakage of stool (fecal incontinence) or leakage of stool and gas (anal incontinence).
- Anal sphincters: Two muscles (external and internal sphincters) that form a band around the anus and allow you to hold in gas and stool.
- Perineum: The tissue (skin and muscles) located between the vagina and the anus.
- Perineal tear: Tearing of the skin and/or underlying muscles of the perineum during vaginal delivery, which sometimes involves the anal sphincter.
- Pelvic floor muscle exercises (PFME): Exercises that strengthen the muscles of the pelvic floor. Regular daily exercising of the pelvic muscles can improve and even prevent urinary and bowel leakage.
- Sacral nerve stimulation: Implantation of a small device near the spinal canal that sends small electrical pulses to the nerves in the anal region, leading to improved control over the bowels. This can also be used to treat urinary leakage.
DIETARY CHANGES
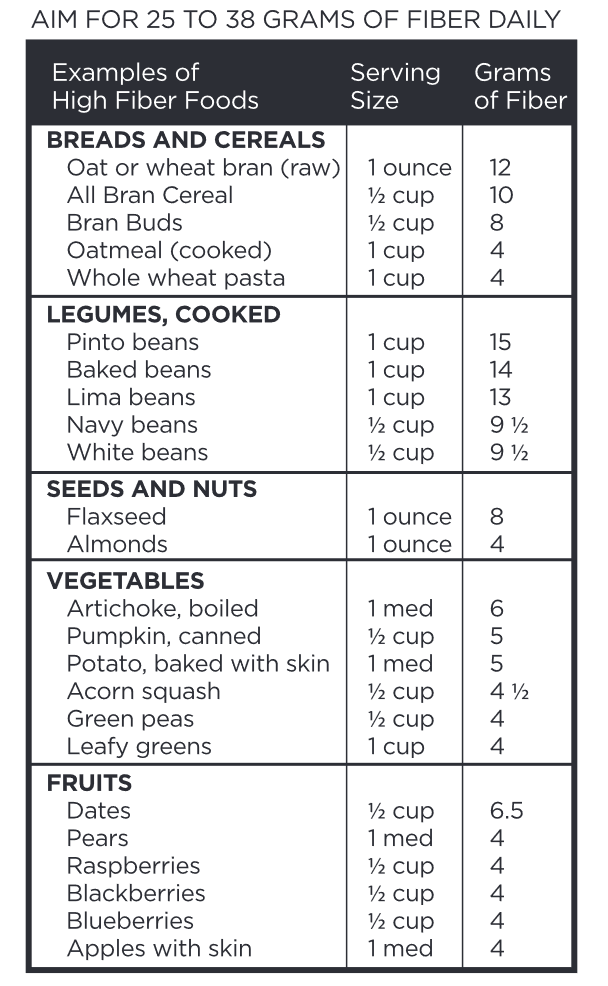
What you drink and eat affects your bowel movements. Drink enough water to make your urine a pale yellow color, but not completely clear like water. Limit caffeinated coffees, teas, and sodas, as well as alcohol and artificial sweeteners. For those with leakage of liquid stool, using fiber to add bulk to your stool can minimize leakage episodes. Avoid constipation and keep stools the consistency of toothpaste. Some women find it helpful to keep a food diary to identify which foods are most bothersome. If you need help figuring out what to eat, ask for a referral to a dietitian.
TIMED BOWEL MOVEMENTS
Eating food stimulates the colon to release stool. Reserve time for a bowel movement after each meal and ensure you can get safely to a bathroom. You also want to have plenty of time to go without having to strain to force a bowel movement out.
SKINCARE
Women with ABL often have sore skin around the anus. Sometimes, this area can become inflamed. Contact your doctor if open sores form. After you go, gently wipe with soft toilet paper, avoiding excessive cleaning. Even better, clean the area with warm water and pat dry. Do not wipe aggressively as this can stimulate stool seepage from the anus. Wearing cotton underwear and loose-fitting clothing is helpful, too. Use cotton pads rather than menstrual pads, if you need a pad. Do not use perfumed or scented soaps, lotions, powders or deodorants-they can worsen the soreness. Other products to avoid include antiseptics, disinfectants, and wipes with alcohol.
PELVIC FLOOR MUSCLE EXERCISES (PFME)
PFME can help manage ABL episodes. For some, strengthening the pelvic floor can stop bowel leakage. Ask your doctor for a referral to a specialized physical therapist (PT) to learn how to best perform PFME. The PT can also teach you exercises to help strengthen your anal muscles.
MEDICINES
The drug loperamide may be taken to help reduce the frequency of diarrhea. Some women with ABL are not able to completely empty their bowels. A laxative may help resolve this symptom. To avoid worsening your problem, talk with your provider before you start using these medicines.
BULKING PROCEDURES
Your surgeon will inject gel just under the wall of the anus to press the walls of the anus together. By narrowing the opening of the anus, the sphincter muscles may be able to close better to hold in the stool.
SACRAL NERVE STIMULATION
For women with leakage of formed stool, sacral nerve stimulation may help gain control over the bowels. A device is implanted in the buttock with the lead extending into the spinal canal to deliver pulses of electricity to the nerves that go to your bowels. This often feels like a faint vibration or tapping sensation. By changing the nerve messages to the bowels, the leakage can be treated.
SURGERY
If the damage to your anal muscles or nerves is severe, surgery may be recommended. There are different types of ABL operations:
- Anal sphincteroplasty: A torn anal sphincter muscle is sewn back together.
- Endoscopic radiofrequency (heat) therapy: The surgeon tightens the anal sphincter muscles by using heat to build up the opening, which helps to control bowel movements.
- Ostomy: As a last resort, the surgeon may suggest that the bowels empty through an opening (ostomy) on your abdomen rather than through the anus.
OTHER OPTIONS
Ask your doctor about anal or vaginal inserts that might help hold in the stool.