If you are experiencing urinary leakage, pelvic floor muscle exercises (Kegels) and bladder training are two things you can do to help control your urinary symptoms.
Pelvic Floor Muscle Exercises
Learning how to strengthen the pelvic floor muscles can help reduce or stop urine leakage. Pelvic floor muscle exercises (PEME) are most helpful for women with mild to moderate urine leakage. Women with severe urine leakage often need more than exercises to improve.
Like any other form of exercise, it is important to do PEME correctly and regularly. Unfortunately, because pelvic muscles are hidden from view, it is hard to know if you are doing them correctly. To be sure that you are working the right muscles:
• Imagine that you are going to pass gas and squeeze the muscles that would prevent that gas from escaping from your rectum. Exercising the muscles around the rectum will also strengthen those around the vagina and under the bladder.
• Use a hand mirror to look at your vaginal opening and the perineum (the space between the vagina and rectum). You should see the perineum lift up when you contract your pelvic muscles.
• While lying or sitting, place one finger inside your vagina. Squeeze as if you were trying to stop urine from coming out. You should feel your finger lifted and squeezed if you are correctly contracting your pelvic muscles.
• No one should be able to tell you are doing PFME – if you are visibly moving, you are not using the right muscles.
• You should not be contracting the gluteus (“butt”) or thigh muscles.
Keep your stomach and back muscles relaxed as you work those pelvic muscles. And, do not squeeze your legs together or hold your breath while doing the exercises. Try this routine:
1. Start by pulling in and holding a pelvic muscle squeeze for 3 seconds, then relax for an equal amount of time (3 seconds).
2. Do this for 10 repetitions three times a day.
3. Try to hold for 1-second longer each week until you are holding for a 10-second squeeze.
4. Remember to rest and breathe between contractions. Relaxing can be as important as squeezing.
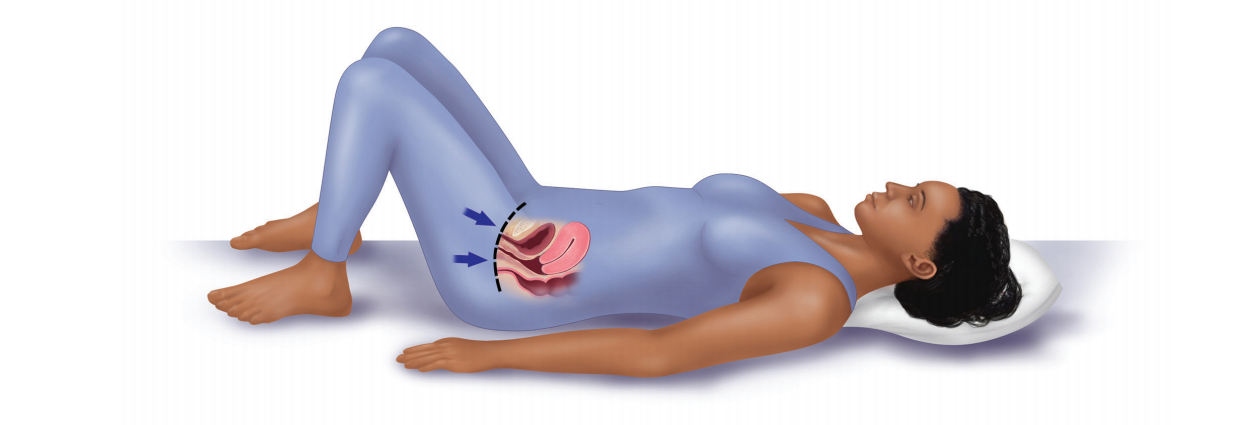
5. At the beginning, do the exercises while lying down. As you get stronger, you should do the exercises while sitting or standing.
If you are not sure that you are doing the exercises correctly, ask your medical provider during a pelvic exam to check if your squeezing is working the right muscles. You can also ask for a referral to a physical therapist who specializes in pelvic floor muscle rehabilitation. The physical therapist will also check your back and abdominal strength, your gait as well as your posture. These all affect how your pelvic muscles work.
About Bladder Training
Now that you’ve got the right muscles and good strength, it’s time to put that muscle to work!
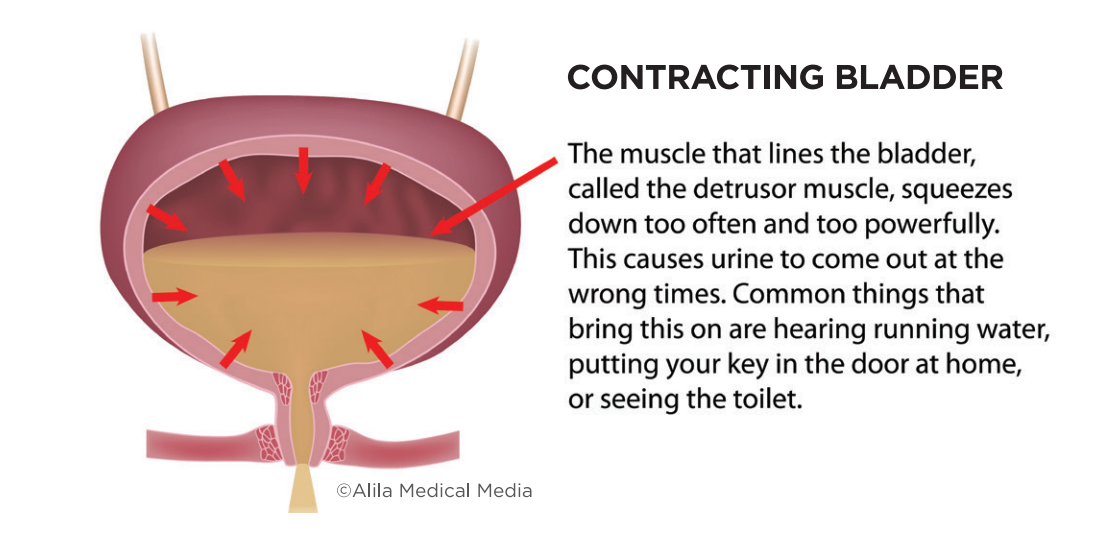
Normally, the bladder can hold urine for 2 to 4 hours–then you feel the urge to urinate–and should be able to walk to the bathroom and urinate normally. Women with overactive bladder (OAB) feel a sudden and immediate urge to urinate. This is called urgency. This urgency may lead to urine leakage. Bladder training can help hold the urine longer and overcome that gotta-go sensation without medicines or surgery.
Bladder training programs involve urinating on a schedule. Over time, you increase the time between bathroom trips. This helps to increase the amount of urine that your bladder can hold. The goal of bladder training is to feel less need to rush to the bathroom frequently. Here are the steps to better bladder control:
STEP 1: Talk with your provider about your bladder symptoms. Get checked for a bladder infection or other health issues that can cause these symptoms. Keep a bladder diary. Write down the time when you urinate, how much you urinated, as well as what and how much you drink. Also, log every time you feel the need to go.
STEP 2: Review the diary with your provider and decide on the best approach to bladder training. Commit to get your bladder in shape, either on your own or with help. Research shows bladder training reduces frequency and urgency. But, just like other exercise programs, bladder training requires motivation. With practice, this will get easier. Ask about working with a physical therapist if you think that would help you.
STEP 3: Make a training schedule. Most women start by urinating every 30 to 60 minutes during the day, whether or not they feel the need to go. If you get the urge to go before the scheduled time, do not run to the bathroom. Try some of the following strategies:
- Practice your PFME squeeze as explained above. This helps to close off the urethra preventing urine from leaking. Continue to squeeze until the need to go fades. Another option is to quickly squeeze and release the muscles, distracting the bladder from squeezing.
- Cross your legs or sit on a hard surface.
- Distract your mind. Count backward from 100.
- Shift your position. You might find that leaning forward helps to settle your bladder.
STEP 4: After 1 to 2 weeks, if you are not having leaking accidents, increase the time between bathroom trips by 30 minutes. Stop making those “just in case” visits to the bathroom.
STEP 5: Be patient and stick with it. You may notice improvement within a couple of weeks; however, the bladder retraining period can take several months. Below are additional tips to help make your bladder training a success:
- Maintain normal body weight. If you are overweight, losing a small amount of weight (even 10% of what you weigh) can help with bladder leakage. Extra weight can increase the urge to go.
- If you smoke, quit. Smoking can lead to lung problems, which make you cough often. Coughing can promote urinary leakage. Nicotine can also cause bladder spasms.
- Treat constipation. Constipation can make overactive bladder and urine leakage worse.
- Learn about the side effects of your medicines. Ask your provider if any of your prescribed or over-the-counter medicines might be worsening the gotta-go feeling. Diuretics (water pills are one example of a prescription medication that may have this effect.) If so, discuss alternate options.
- Drink when you are thirsty, but do not overdrink. Drink only enough so that your urine is a light yellow color. Spread your drinks across the day to help control your need to urinate.
- Stop drinking two hours before you go to bed. This will help to decrease your need to get up during the night to use the bathroom.
- Stop or limit any drinks that irritate your bladder. This can include drinks with alcohol, caffeine, artificial sweeteners, or diet drinks.
THREE TAKEAWAYS
1. By exercising your bladder and pelvic floor muscles, you can help control the urge to urinate.
2. Bladder training is effective for many women-stick with your schedule and give yourself time to relearn when to respond to the need to go. This can mean you avoid medicines and surgery.
3. When done correctly, pelvic floor muscle exercises can help reduce or stop urine leakage. If you are unsure about your technique, ask for a referral to a pelvic floor physical therapist.