Interstitial cystitis/bladder pain syndrome (IC/BPS) is a condition with symptoms including burning, pressure, and pain in the bladder along with urgency and frequency.
About IC/BPS
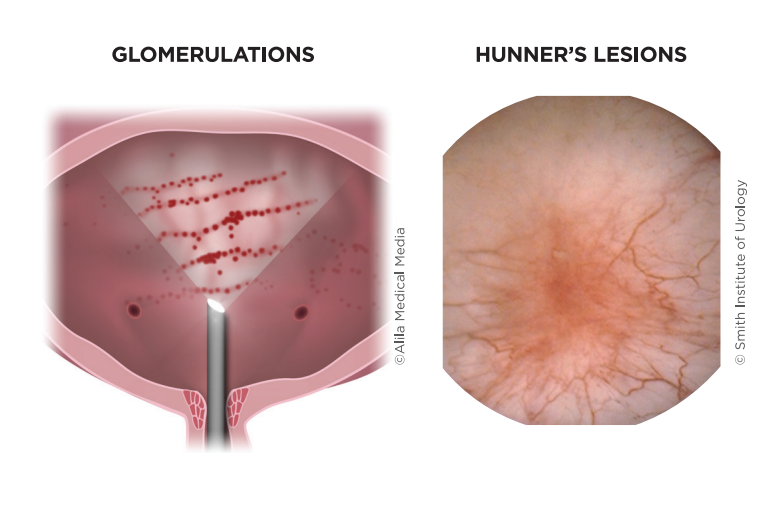
IC/BPS occurs in three to seven percent of women but can affect men as well. Typically this condition–which is often the result of glomerulations and/or Hunner’s Lesions in the bladder–is diagnosed among women in their 40s. Still, younger and older women have IC/BPS too. The condition feels like a constant bladder infection. Symptoms may become severe (called a “flare”) for hours, days, or weeks and then disappear. Or, they may linger at very low levels during other times.
Individuals with IC/BPS may also have other health issues such as irritable bowel syndrome, fibromyalgia, chronic headaches, and vulvodynia. Depression and anxiety are also common among women with this condition.
The cause of IC/BPS is unknown. It is likely due to a combination of factors. IC/BPS runs in families and so may have a genetic factor. Your doctor may perform a cystoscopy to determine if there is damage to the bladder wall. This damage may allow toxins from the urine to seep into the bladder lining’s delicate layers, thus causing the pain of IC/BPS. Other research found that nerves in and around the bladder of people with IC/BPS are hypersensitive. This may also contribute to IC/BPS pain. There may also be an allergic component.
The IC/BPS Bladder
Symptoms of IC/BPS vary from woman to woman. However, most experience pain, pressure, and discomfort as the bladder fills. In addition, chronic pain or pressure in the pelvis and perineum are common, including discomfort and pain during sexual intercourse. The severity of symptoms is variable.
Urinary urgency (“gotta go right now”) and urinary frequency (“gotta go often”) are common during both the day and at night. Many women feel a constant need to empty their bladders to relieve the intensity of the pain. Women with IC/BPS rarely leak urine but often go to decrease pain. IC/BPS flares are common during the menstrual period. Flares also occur during times of emotional or physical stress. Some women note symptoms specifically in their urethra. For them, urinating can feel like pushing sharp pieces of glass into the tissue.
When cystoscopy is performed on women with IC/BPS, the bladder appears inflamed and irritated. Often pinpoint sites of bleeding, called glomerulations, can be seen on the bladder wall. A small number of women have a specific type of lesion known as Hunner’s lesion. Cracks in the lining of the bladder are also often visible.
DIAGNOSIS
To diagnose IC/BPS, your urologist or urogynecologist will review your medical history and symptoms. Your doctor will ask about your pattern and level of pain, as well as urinary symptoms. You may need some lab tests to help rule out other conditions. Cystoscopy and urodynamics testing may be done depending on your symptoms but are not required. Often you will be asked to keep a diary of your bladder symptoms, urinations, and fluid intake.
Women diagnosed with IC/BPS typically experience pain, burning, pressure, and discomfort in the bladder for more than six weeks with no other apparent cause. Some women go years with these symptoms before seeking treatment and receiving the correct diagnosis.
TREATMENTS
Treatments depend on the severity of symptoms. Most women require more than one type of therapy to manage their pain and urinary symptoms. At this time, there is no cure for IC/BPS, but the symptoms can be treated and controlled.
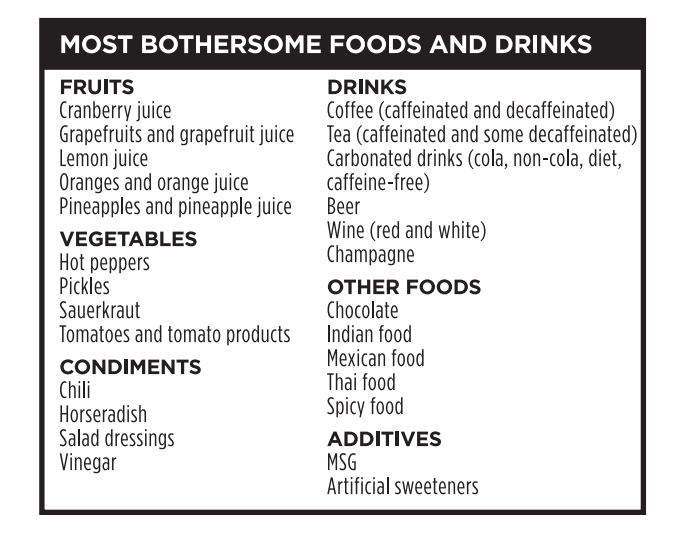
DIET: Women with IC/BPS often find that certain foods and drinks irritate their symptoms. Identifying which items are bothersome to you and restricting or limiting them can help control symptoms. Food sensitivities can vary. However, some foods and beverages seem to trigger a flare among many women. Often women eliminate these foods and slowly add them back individually to determine which ones they can still eat safely. It’s helpful to meet with a registered dietitian nutritionist to identify individual trigger foods.
STRESS MANAGEMENT: For most women, stress can worsen IC/BPS symptoms. Find an activity that relaxes you. It might be meditation, yoga, hypnosis, acupuncture, or taking a walk. Whatever it is, schedule time so you can help manage stress.
PHYSICAL THERAPY: A specially trained physical therapist (PT) can manually maneuver your pelvic area to help relieve pelvic pain. This therapy may loosen tight pelvic floor muscles and tissues. Women with IC/BPS should NOT do pelvic floor strengthening exercises (called “Kegel exercises”) unless under a PT’s care. These exercises can worsen symptoms.
MEDICINES: Your provider may prescribe one or a combination of medicines. Pentosan polysulfate sodium (ElmironTMM) is the only FDA-approved oral medicine for IC/BPS. It helps about one-third of women control their symptoms. Other drugs that help IC/BPS symptoms include phenazopyridine, amitriptyline, cimetidine, or hydroxyzine.
BLADDER INSTILLATIONS: Some find it helpful to get medicine inserted directly into their bladders. A series of these instillations is usually done in the office. Treatments can be 1 to 2 times a week for 6 to 8 weeks.
CYSTOSCOPY UNDER ANESTHESIA: Stretching the bladder wall, called hydrodistension, can also be helpful. Because this can be painful, it is often performed as an outpatient surgery with general anesthesia. This procedure provides relief for some women. But, it often causes a flare immediately afterward.
NEUROSTIMUATION: Electrical stimulation devices can be placed outside of your body (TENS unit) or surgically implanted inside the body (called InterStim®). They send mild electrical pulses through the pelvic area. This can help relieve IC/BPS symptoms, especially urinary symptoms.
BOTULINUM TOXIN (BOTOX): Botox can increase bladder capacity, helping a patient with IC/BPS urinate less often. Your doctor uses a small camera and needle to inject Botox into the bladder wall under local anesthetic or sedation. Typically, the injection needs to be repeated 1 to 2 times per year. A small number of women experience side effects, such as difficulty emptying the bladder or urinary tract infection.
SURGERY: Surgery is reserved for extreme cases as most women never need surgery. For women with Hunner’s lesions, the area can be surgically treated with a laser. Very rarely, the bladder may be surgically enlarged or removed entirely.
THREE TAKEAWAYS
1. Interstitial cystitis bladder pain syndrome CIC/BPS) is a condition characterized by bladder pain, pressure, and discomfort along with urinary urgency and frequency, without any sign of infection or other cause.
2. Treatments often Include diet changes, stress management, physical therapy, medicines, bladder installations, cystoscopy under anesthesia, nerve stimulation, and Botox injections.
3. A bladder diary can help provide more information about the link between diet and your bladder symptoms.