Sacrocolpopexy is an operation to correct uterine prolapse or to correct vaginal vault prolapse in women who have had a hysterectomy. This surgery offers long-term treatment of apical prolapse with success rates greater than 80 percent.
About Sacrocolpopexy Surgery
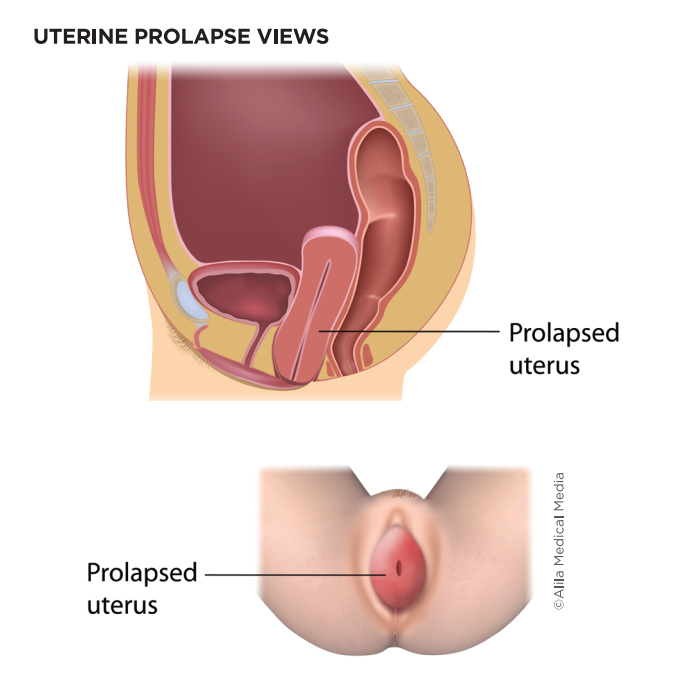
When the upper support of the vagina weakens, a woman may experience uterine prolapse; that is, the uterus and cervix drop into the vaginal canal. Women who have had a hysterectomy may experience vaginal vault prolapse, which is when the top (apex) of the vagina drops into the vaginal canal. Both conditions may cause a sense of pressure and a bulge at the opening of the vagina. For symptomatic women, treating a prolapse using a pessary or surgery can restore normal anatomy and fix symptoms. One surgical option is sacrocolpopexy.
The success rate for this operation is very high. However, for a small percent of women, the vaginal vault prolapse may recur. In addition, like any surgery, there are risks to sacrocolpopexy:
- Slow return of normal bladder emptying requiring the temporary use of a catheter in about half of women.
- Slow return of normal bowel function.
- Bladder or urinary infections.
- Infection of the skin incisions made during surgery. This is less common with small incisions with laparoscopic surgery compared to a larger incision.
- Blood clot formation in the legs (deep vein thrombosis-DVT) or lungs (pulmonary embolus-PE).
- Pelvic pain, including pain with sex.
- Exposure of the mesh in the vagina, which sometimes can be treated in the office but may require more surgery.
- Changes in urination (slow urine stream, for example).
- Changes to bowel movements.
- Injury to nearby organs, including the bowels, bladder, ureter (the tube from the kidney to the bladder), vagina, nerves, or large blood vessels in the pelvis.
- Women rarely need a blood transfusion after this surgery.
Ensure you have all your questions answered ahead of time and know how to contact your surgeon with questions or problems after surgery.
For more about preparing and recovering from urogynecological surgeries, ask your doctor’s office for a copy of the “Surgery: What to Expect” fact sheet.
How the Surgery is Done
This surgery requires general anesthesia. This means you will be asleep during the operation with a breathing tube in your throat.
The operation is performed through a larger incision on your abdomen or laparoscopically through small incisions. Laparoscopic surgery may be performed with the use of a surgical robot as well. You will have a catheter placed in your bladder in the operating room after you are asleep.
LEARN THE TERMS
- Apical prolapse: Generic term for prolapse of the top of the vagina or uterus.
- Catheter: The plastic tube that is placed temporarily in the urethra and up into the bladder to drain urine from your bladder.
- Hysterectomy: Surgical removal of the uterus. Note that hysterectomy does not always include the removal of the ovaries. Removal of ovaries is a different surgery called oophorectomy, which can be performed at the same time as a hysterectomy.
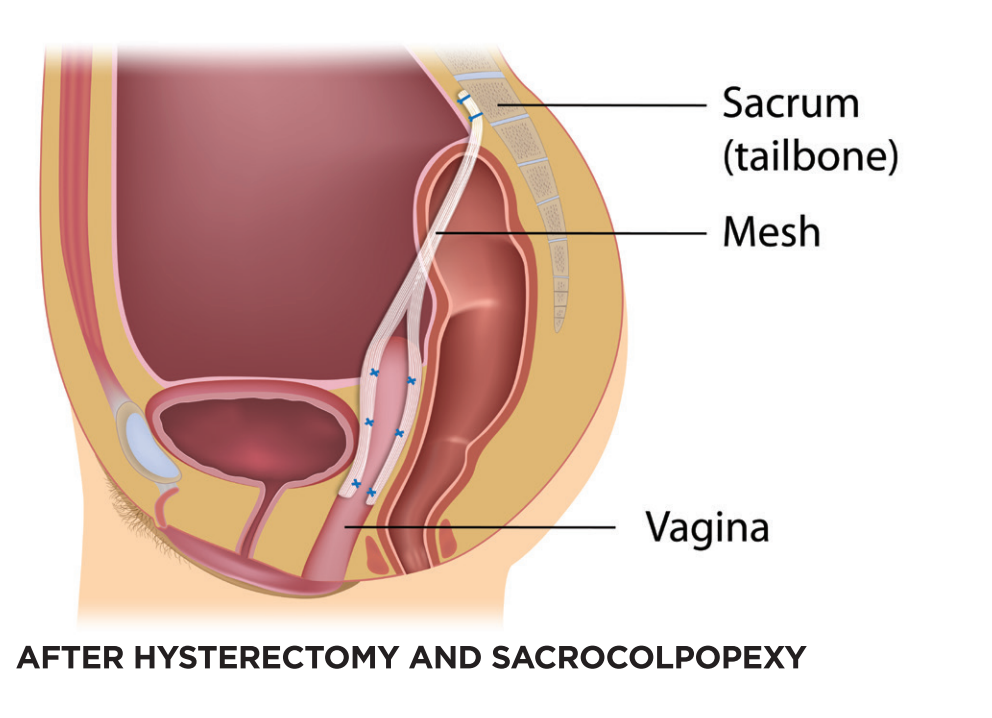
- Sacrocolpopexy: An operation to correct uterine prolapse or vaginal vault prolapse in which the vaginal walls are connected to a Y-shaped piece of mesh material that is suspended from the sacrum (tailbone).
- Sacrum: The bones at the base of the spine, also called the tailbone.
- Supracervical hysterectomy: The uterus is removed, and the cervix is left in place.
- Synthetic mesh material (or mesh): A medical-grade plastic called polypropylene that is used in some incontinence and prolapse surgeries, which is permanent.
- Total hysterectomy: The uterus and cervix are removed.
- Uterine prolapse: The supports to the uterus and upper vagina weaken, allowing the uterus to slide down into the vagina canal or beyond the vaginal opening.
- Vaginal vault prolapse: Upper support of the vagina weakens in a woman who has had a hysterectomy, allowing the vaginal walls to sag into the vaginal canal or beyond the vaginal opening.
If you still have a uterus, your surgery may include a hysterectomy and possible removal of the tubes (salpingectomy) or ovaries (oophorectomy). A portion of your cervix may be left in place, which is called a supracervical hysterectomy. Ask your doctor about the specific portions of your surgery.
During a sacrocolpopexy, the surgeon carefully separates the vaginal walls from the bladder and the rectum. The surgeon then attaches a Y-shaped piece of permanent mesh to both the front and back walls of the vagina as well as the top of the vagina (or cervix if it is still present). The mesh is then suspended to a ligament running down the front of the sacrum, which is the base of the spine near the tailbone. The mesh is firmly sutured in place, restoring the vagina to its normal position. This also supports the bladder and bowels. The surgeon carefully covers the mesh with a layer of tissue.
The mesh material used in this surgery is permanent and will not dissolve over time. It is made of a suture material called polypropylene, which has been used in surgery for many years, woven into a fabric. While all surgery carries some risks, mesh placed during sacrocolpopexy has a lower risk of complication than if the mesh is placed through the vaginal opening to fix prolapse.
Other operations to correct pelvic floor disorders may be done at the same time, such as procedures to address urinary incontinence. The surgeon will also look inside your bladder with a small camera to ensure nothing was damaged.
After the operation, you will be in a recovery room for a couple of hours. When you wake up, the catheter will be in your bladder, and you may have gauze material in the vagina. The gauze will be removed, and then your bladder will be tested to see if it is ready to empty on its own before you leave the hospital. As many as 50 percent of women have trouble emptying the bladder immediately after this surgery. These symptoms are usually temporary. You may need to go home using a catheter, either placing one yourself intermittently or having it in place all the time. If so, a nurse will teach you how to do this. Ask your surgeon about when you can stop using the catheter.
Discharge Considerations
Your hospital stay depends upon the way the surgery is performed. For example, larger incisions typically require a two to a three-day hospital stay. With laparoscopic or robotic sacrocolpopexy, most patients go home the same day or the next morning.
Most women recover well from this surgery and find relief from their prolapse symptoms. Give yourself time to heal over the next six to eight weeks. You may notice spotting and discharge from your vagina. This is normal. If the discharge has a foul odor or there is heavy bleeding, call your doctor’s office. Constipation is also prevalent after surgery. You will likely need the help of stool softeners and laxatives for a short time.
Avoid lifting anything too heavy to lift easily with one hand for six to eight weeks after surgery. You can do light activities, and walking is good for you. Don’t stay in bed all the time, but refrain from high-impact activities, swimming, spa baths, and sexual intercourse. Once you feel your reflexes are back to normal and you are not using narcotic pain medicines, you can drive.
Ask your surgeon when you should schedule a post-operative appointment. Discuss at that visit when to resume your regular activities.
THREE TAKEAWAYS
1. Sacrocolpopexy is an operation to correct uterine or vaginal vault prolapse. This surgery has a high success rate of 80 percent.
2. The operation is done under general anesthesia and requires the use of permanent synthetic mesh material. The surgery may be performed using a larger abdominal incision or small laparoscopic incisions.
3. Most women recover well from this surgery in six to eight weeks. Avoid heavy lifting after surgery for six weeks. It is normal to notice spotting and white or yellow discharge from your vagina. You may need to use a urinary catheter temporarily. Use stool softeners and laxatives to keep your bowels soft and regular.