About Vaginal Repair with Mesh/Biological Graft
Pelvic organ prolapse is a dropping or drooping of the pelvic organs, such as the bladder, vagina, uterus, and rectum, caused by a loss of pelvic support. Women with prolapse experience symptoms including pelvic pressure and a vaginal bulge. One option for treating these issues is prolapse is surgery. The goal of this surgery is to rebuild vaginal supports that have been lost over time.
Prolapse surgery is different from a surgery designed to remove an organ like the uterus or gallbladder—those surgeries are successful simply when the organ is removed. When surgery is designed to repair weakened tissue, it is not always successful over time. In one of three women who has had prolapse surgery, the organs drop again in the same or a different part of the vagina. Factors that may contribute to prolapse recurrence include the type and severity of prolapse, age, obesity, chronic cough, constipation, and regular heavy lifting.
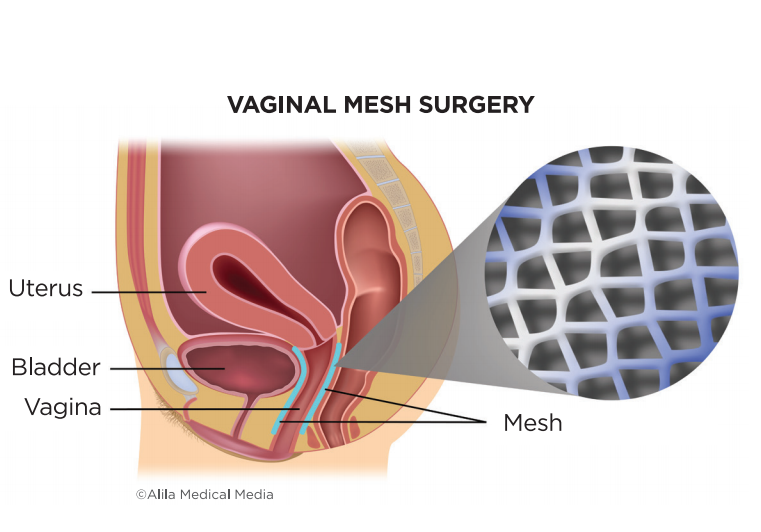
The most challenging type of prolapse to repair is a dropped bladder. Research has found that using a synthetic permanent mesh implant to reinforce bladder prolapse repair is more effective over time than traditional surgery using a woman’s own tissue and stitches. The mesh provides extra support for the vaginal walls, bladder, uterus, or bowel. This helps to prevent the organs from dropping again.
The long-term effectiveness of mesh surgeries is still being evaluated, as well as the impact of some of the side effects of surgery. Thus, there are varying views among doctors about mesh. Some surgeons only use mesh for certain patients. This often includes women who had prolapse surgery before and the prolapse has come back. Others may recommend it for women with a large prolapse or those at high risk for recurrent prolapse.
Like most surgeries, there are risks of mesh and graft implant use. In some women (10 to 15 percent), the mesh may become exposed through the vaginal wall. This is often called erosion or extrusion. In this case, you or your sexual partner might feel a scratching sensation. Your doctor can often see the exposed mesh during a pelvic exam. Plus, it may cause vaginal spotting or discharge. Treatment options to correct this problem include low-dose vaginal estrogen or surgery. Mesh has also been found later in the bladder or bowel of women who have had prolapse surgery, which requires additional surgery.
Some women who have had mesh surgery experience pain and muscle spasms afterward. This can occur during sex or just at rest. Sometimes this requires the mesh to be removed. In severe cases, the symptoms do not completely improve after mesh removal because of scar tissue and muscle spasms. Other treatments for this problem include medicines, injections of numbing medicines, or physical therapy.
Vaginal mesh surgery should only be done by a surgeon who has received specialized training in these procedures. Find a surgeon who can repair your problem with or without mesh—then talk about which is best for you.
Before the surgery, ask your doctor to explain the procedure, including the benefits and the risks. Discuss potential health conditions that increase risks, such as smoking, diabetes, and atrophy.
Make sure you have all your questions answered ahead of time and know how to contact your surgeon with questions or problems after surgery.
For more about preparing and recovering from urogynecological surgeries, ask your doctor’s office for a copy of the “Surgery: What to Expect” fact sheet.
How the Surgery is Done
During prolapse surgery, the surgeon positions the mesh implant in the vagina through incisions in the vaginal walls so that it holds up the drooping or dropped organs. You may also have some small incisions on the outside of the vaginal area. Your surgeon may tailor the piece of mesh for your specific anatomy or use a preformed “mesh kit” package. If your surgeon uses a synthetic permanent mesh, body tissue will grow through the holes, and the mesh will slowly become part of your body. In contrast, after 6 to 9 months, biological grafts are typically absorbed and replaced with your own body tissue.
Discharge Considerations
After you go home, ask someone to stay a few days or visit with you frequently if you live alone. Expect to feel more tired than usual.
Most women recover well from this surgery and find relief from their prolapse symptoms. Give yourself time to heal over the next six weeks. You may notice spotting and discharge from your vagina. This is normal. If the discharge has a foul odor or there is heavy bleeding, call your doctor’s office. Constipation is also prevalent after surgery. You will likely need the help of stool softeners and laxatives for a short time.
Avoid lifting anything heavier than you can easily lift with one hand. You can do light activities, and walking is good for you. Don’t stay in bed all the time, but refrain from high-impact aerobic exercises, swimming, or spa baths. Once you feel your reflexes are back to normal and you are not using narcotic pain medicines, you can drive.
Ask your surgeon when you should schedule a post-operative appointment. Discuss at that visit when to resume your regular activities.
Three Takeaways
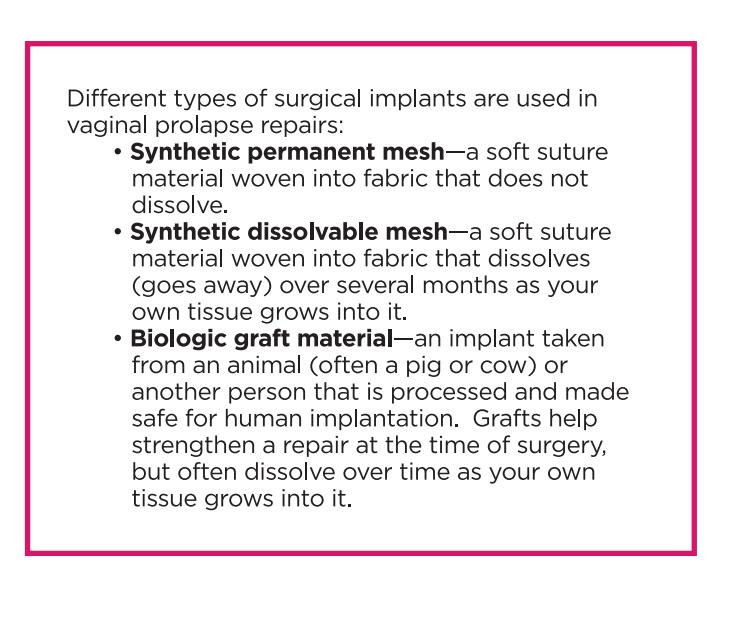
1. Not all mesh is the same. Some mesh is permanent, while other types of mesh dissolve. Success rates for vaginal prolapse repair with mesh depend on the type and severity of prolapse and the type of implants used.
2. Erosion of the mesh into the vagina happens in about 10 to 15 percent of women who have prolapse repair with synthetic permanent mesh. It can cause pain and bleeding. Treatments include low-dose vaginal estrogen and surgery.
3. Mesh surgery should only be done by a surgeon who has received specialized training on these procedures. Find a surgeon who can repair your problem with or without mesh —then talk with them about which option is best for you.