Colpocleisis, or vaginal closure surgery, is a procedure to correct bladder, uterine, or vaginal vault prolapse. It is done for women who are no longer sexually active, often those who are older.
ABOUT VAGINAL CLOSURE SURGERY
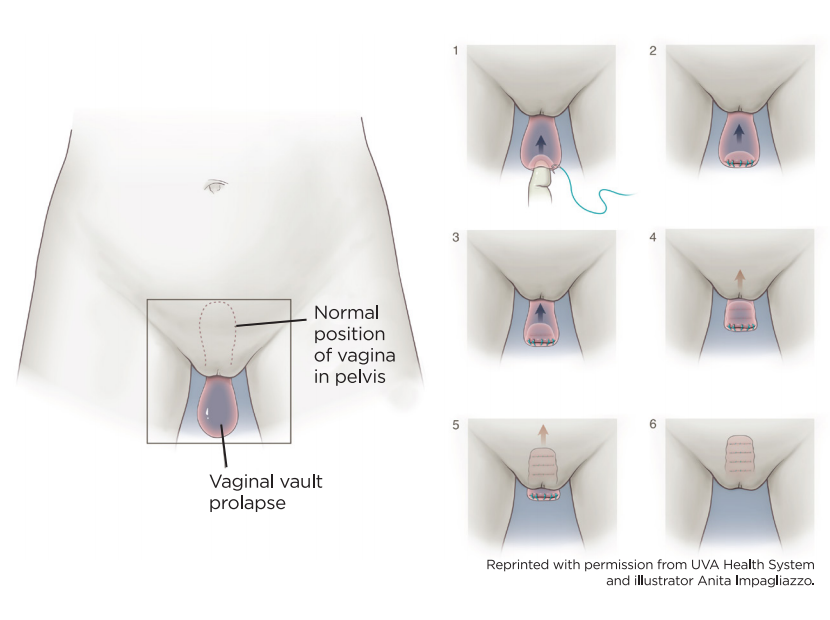
In patients with advanced pelvic organ prolapse, the top of the vagina can protrude out of the vaginal opening. This may happen in women who still have their uterus or in women who have had a hysterectomy. For some women, it may cause ongoing discomfort, bleeding, and trouble emptying the bladder.
If you do not plan to have penetrative vaginal sex in the future, colpocleisis or vaginal closure surgery can be very successful with low risk. The success rate for this type of surgery is about 95 percent. After the surgery, both prolapse symptoms and overall quality of life improve for most women. While any surgery requires recovery time, most women report little pain after colpocleisis.
There are several advantages of this surgery. The surgery is done completely vaginally, without going into the belly cavity. Thus, surgical risks are minimized, and most women heal quickly-the average recovery time is two to three weeks. Plus, most women can go home the same day of surgery or after one night in the hospital.
Like other operations, there are risks associated with this surgery:
- Changes to urination (slowing of the urine stream, urinary incontinence) or bowel movements.
- Bladder infections are a risk for some women.
- Infection of the skin incisions if made during surgery, which may be only on the outside of the vaginal opening.
- Blood clot formation in the legs (deep vein thrombosis-DVT) or lungs (pulmonary embolus-PE).
- Pelvic pain.
- Injury to nearby organs, including the bowels, bladder, ureter (the tube from the kidney to the bladder), vagina, nerves, or large blood vessels in the pelvis.
- Women rarely need a blood transfusion after this surgery.
Make sure you have all your questions answered ahead of time and that you know how to contact your surgeon with questions or problems after surgery.
For more about preparing and recovering from urogynecological surgeries, ask your doctor’s office for a copy of the “Surgery: What to Expect” fact sheet.
DO I HAVE TO HAVE MY VAGINA CLOSED OFF? NO.
If you are interested in having vaginal intercourse (sex) in the future, you should be open and honest with your surgeon about that hope. Ask about alternatives to vaginal closure surgery. Other surgeries will reconstruct a normal vaginal canal and allow for future vaginal intercourse. They are also very safe and successful. Do not feel pressured to have closure surgery if the possibility of future vaginal intercourse is important to you.
LEARN THE TERMS
- Catheter: A plastic tube temporarily placed up through the urethra into the bladder to drain urine from your bladder.
- Cervix: Donut-shaped tissue at the bottom of the uterus, which dilates in childbirth to permit delivery. Pap smears are done to check that cells of the cervix are not cancerous.
- Cystocele (anterior vaginal wall prolapse): Front wall of the vagina sags downward or outward, allowing the bladder to drop from its normal position.
- Colpocleisis: An operation in which the vaginal walls are sewn together to fix vaginal vault prolapse in women who are no longer sexually active. This word means “close vagina” in Greek.
- Hysterectomy: Surgical removal of the uterus. Note that hysterectomy does not always include the removal of ovaries.
- Labia: Folds of skin on either side of the vaginal opening.
- Uterine prolapse or vaginal vault prolapse: Upper support of the vagina weakens, allowing the uterus and cervix to drop into the vaginal canal. In women who have had a hysterectomy, the top of the vagina falls.
- Uterus: The female reproductive organ where a pregnancy grows, sometimes referred to as the womb.
- Vagina: The canal that connects the uterus (womb) with the vulva.
- Vaginal vault prolapse: Upper support of the vagina weakens in a woman who has had a hysterectomy, allowing the vaginal walls to sag into the vaginal canal or beyond the vaginal opening.
- Vulva: A woman’s external genitals.
HOW THE SURGERY IS DONE
This surgery can be done under general anesthesia, which means you will be asleep during surgery with a tube in your throat. It can also be done under spinal anesthesia, which means you would be numb from the waist down but breathing on your own. Discuss these choices with your surgeon, medical doctor, and anesthesia team.
After you are numb or asleep, a catheter will be placed in your bladder.
After you go home, ask someone to stay a few days or frequently visit with you if you live alone. Expect to feel more tired than usual. Most women have little pain.
During the surgery, the surgeon removes the vaginal lining and the internal vaginal walls are sewn together so that the vagina cannot bulge out. Dissolving stitches are placed to sew the front wall of the vagina to the back wall, which pushes the prolapsed organs inside your body and prevents them from falling. Your surgeon may also place some sutures to narrow the vaginal opening to help prevent the prolapse from coming back. No mesh is used during this surgery. Other operations to correct pelvic floor disorders may be done at the same time, such as a hysterectomy or procedures to address urinary incontinence. Your surgeon will also look inside the bladder with a small camera to ensure nothing was damaged.
If you still have a uterus, it will be pushed up above the stitches placed in the vagina. Small drainage tunnels will be created to drain blood or mucus. You may need some tests before surgery to make sure this is safe. These may include a Pap smear, uterine biopsy, or pelvic ultrasound.
After this surgery, the vagina is only about one inch long and the opening is very narrow, which prevents vaginal sex. The outside of the vaginal area, including the labia and vulva, still looks the same. Only the inside is different. Because the outside is the same, external sexual stimulation such as stimulation of the clitoris, the primary organ of arousal in women, is still possible.
After surgery, you will be in a recovery room for a couple of hours. When you wake up, there will be a catheter will be in your bladder. It will be removed, and then your bladder will be tested to see if it is ready to empty on its own before you leave the hospital. As many as 50 percent of women have trouble emptying the bladder immediately after this surgery. These symptoms are usually temporary. You may need to go home using a catheter, either placing one yourself intermittently or having it in place all the time. If so, a nurse will teach you how to do this. Ask your surgeon about when to stop using the catheter.
DISCHARGE CONSIDERATIONS
Colpocleisis can be an outpatient procedure, so depending on other health considerations, you may be able to go home the same day as your surgery. Or, you may stay one night in the hospital.
After you go home, ask someone to stay a few days or frequently visit with you if you live alone. Expect to feel more tired than usual. Most women have little pain.
Most women recover well from this surgery and find relief from their prolapse symptoms. Give yourself time to heal over the next six weeks. You may notice spotting and discharge from your vagina. This is normal. If the discharge has a foul odor or there is heavy bleeding, call your doctor’s office. Constipation is also very common after surgery. You will likely need the help of stool softeners and laxatives for a short time.
Check with your surgeon about lifting and activity after surgery. You can do light activities, and walking is good for you. Don’t stay in bed all the time. Once you feel your reflexes are back to normal and you are not using narcotic pain medicines, you can drive.
Ask your surgeon when you should schedule a postoperative appointment. Discuss at that visit when to resume your regular activities.
THREE TAKEAWAYS
1. Colpocleisis is an operation to close off the internal vaginal canal to correct pelvic organ prolapse in women who are no longer sexually active. The success rate for this surgery is about 95 percent.
2. After the surgery, the outside (vulva, urethral, and anal openings) looks the same, but the vagina is shorted and narrowed. Vaginal intercourse (sex) Is not possible.
3. The operation is done in the hospital and may require a one-night stay. Since the surgery requires only a vaginal incision, most women heal quickly and with little pain. It may take you six weeks to get all your energy back.