Overactive bladder (OAB) is a complex condition affecting about 15 percent of women of all ages. It can be costly, embarrassing, and result in avoiding social activities for fear of leakage. Age increases the risk for OAB, as do some bladder conditions (infection, bladder stones, or abnormal growths). For some women, the cause is unknown.
The Overactive Bladder
Women with OAB feel a sudden urge to urinate, sometimes followed by leaking. Some women leak on the way to the bathroom or while they are pulling down their clothes. Sometimes the whole bladder empties. It is common to feel the frequent urge to go even though your bladder isn’t full.
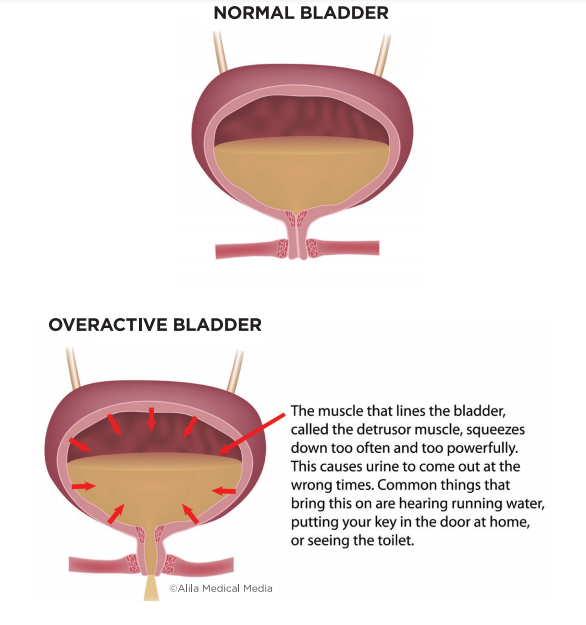
Made of muscle, the bladder walls hold urine. As urine flows into the bladder, the walls expand to make room for more fluid, like a water balloon. The muscles that surround your urethra, the tube you urinate from, tighten to hold in urine while the bladder muscle relaxes.
In women with OAB, the bladder muscle is overactive and squeezes too often. These bladder spasms make it feel like you need to urinate often and quickly, even if there isn’t much urine in your bladder.
DIAGNOSIS
It can feel embarrassing to have these bladder issues. You are not alone. As a first step to taking back your life, talk to your medical provider or bladder specialist, like a urogynecologist or urologist. Discuss when and how often you leak urine. A physical exam helps identify other conditions that influence the bladder, such as prolapse.
Additional tests might include:
• Urine analysis to check for a urinary tract infection and blood in your urine.
• Ultrasound to assess how much urine remains in your bladder after urinating.
• Urodynamics testing to provide information on your bladder and urethra.
You may be asked to complete a bladder diary. This requires you to record what, how much, and how often you drink. You also measure the amount you urinate. This will help your provider learn more about your bladder symptoms.
TREATMENTS
Ask about the best treatment or combination of therapies for you. You can control OAB, and you can get your life back.
DIETARY CHANGES. Certain types of drinks can provoke bladder spasms. For example, coffee, tea, sodas, and other beverages with caffeine worsen symptoms. Artificial sweeteners, fruit juices, and alcohol can also bother your bladder. Completing a bladder diary can help you look for a connection between your diet and bladder symptoms.
PADS AND SKINCARE. The goal of OAB treatment is to reduce leakage. In the meantime, use only all-cotton or incontinence pads (not menstrual pads), as they are gentle on the skin. Try to let the skin air out and dry when possible. Some women need to use a barrier cream to protect the skin near the vagina.
BLADDER TRAINING. Women with OAB tend to go to the bathroom often. However, this can make symptoms worse. Your bladder learns to hold less urine, leading to even more frequent bathroom trips. Bladder re-training involves using your pelvic floor muscles and “mind over bladder” techniques to gradually increase the time between bathroom visits. As you do this more and more, your bladder muscle readjusts. This allows you to make fewer bathroom trips.
This retraining can be hard to do. Ask your doctor for a referral to a pelvic floor physical therapist (PT) to learn how to do it.
MEDICINES. OAB medicines help your bladder hold more urine for longer periods of time. They also reduce urine leakage. Potential side effects include dry mouth and constipation. There are many different medicines available. Let your doctor know how the drugs work for you. It may take trying different medicines before you find the one that works best for you.
PELVIC FLOOR PHYSICAL THERAPY. Most women find that pelvic floor muscle exercises help improve symptoms. For the best effect, work with a specialized PT to learn the techniques. Ask your provider for a referral. Then use these exercises every time you feel a sense of urgency. It may take 3 to 6 months of regular pelvic floor muscle exercise to see results.
BOTULINUM TOXIN (BOTOX). Botox relaxes the bladder muscle. This allows more urine to be held in the bladder before you have to go to the bathroom. Under a local anesthetic or sedation, your provider uses a small camera and needle to inject Botox into the bladder wall.
Typically, the injection needs to be repeated 1 to 2 times a year. A small number of women experience side effects, such as difficulty emptying their bladder or urinary tract infection. Ask your provider if Botox is right for you.
NERVE STIMULATION. There are many nerves involved in bladder function. Nerve stimulators help control these nerves reducing the need to urinate often.
- Tibial nerve stimulation is similar to acupuncture. A small needle is inserted near a nerve in the ankle and connected to an external device that delivers small pulses to the nerve. This changes the messaging to the bladder. This is done during a series of office visits.
- Sacral Nerve Stimulation is a device surgically implanted near the spine. It modulates the bladder nerves.
THREE TAKEAWAYS
1. Bladder spasms can create the need to urinate urgently and often.
2. Diet changes and bladder retraining can reduce OAB. A bladder diary can help provide more information about the link between diet and your bladder symptoms.
3. Treatments, Including physical therapy, medications, Botox, and nerve stimulation, help manage the symptoms.